
Common Risk Factors That Lead to Wound Dehiscence
When an incision or injury begins to separate after it has been closed, that’s wound dehiscence. It lengthens recovery, raises infection risk, and can lead to hernias or, in severe cases, exposed tissue that requires urgent intervention. Understanding why wound dehiscence happens is the first step to preventing it. Most cases trace back to a mix of local stresses at the incision, systemic health factors that slow healing, and care routines that either help or hinder the body’s repair stages. By recognizing risks early, patients and clinicians can make minor adjustments that pay off in faster, safer closure.
How Infection Pushes Wound Dehiscence Off Course
Infection is one of the most common accelerants of separation. Bacteria and biofilm keep inflammation high, degrade collagen, and weaken the bonds that hold an incision together. Even a subtle increase in warmth, redness, or drainage can shift a healing cut toward wound dehiscence if not addressed quickly. Clean technique at home, timely dressing changes, and early evaluation for antibiotics or debridement when indicated control bioburden so regenerating tissue can organize and strengthen rather than unravel.
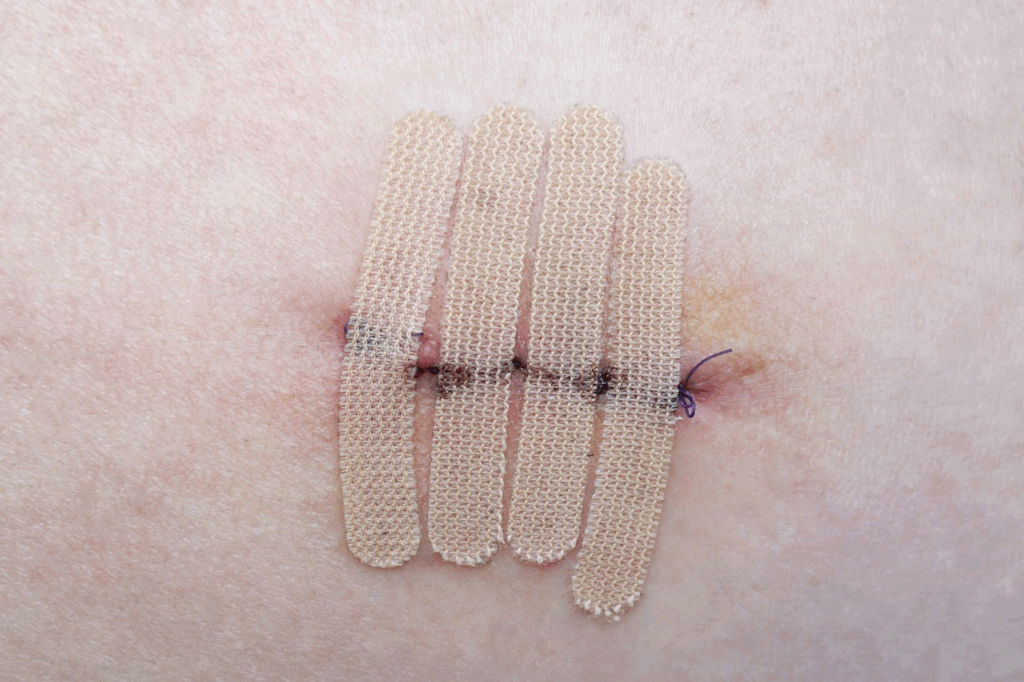
Mechanical Triggers of Wound Dehiscence
Excessive tension pulls on edges like a stretched rubber band; over time, micro-tears give way to visible separation. Technique matters: suture spacing, depth, and material all influence how forces are shared across the line.
Balanced Tension Protects Edges
Evenly distributed bites and appropriately sized sutures help resist daily movement without strangling tissue.
Life Adds Load
Coughing, sudden twists, or lifting something heavy can multiply stress on a vulnerable incision.
Circulatory Links to Wound Dehiscence
Healing is an oxygen-hungry process. When circulation is impaired—by tight dressings, edema, peripheral arterial disease, or significant anemia—the wound bed is starved of the fuel it needs to lay collagen and knit together. Hypothermia and low blood pressure in the perioperative period can compound that deficit. Restoring flow with elevation, edema control, and treatment of underlying vascular issues shifts the biology toward synthesis rather than breakdown, reducing the chance of wound dehiscence as the days pass.
Human Factors in Wound Dehiscence
Advanced age and frailty change skin architecture and slow cellular turnover. Malnutrition, whether from illness, reduced intake, or restrictive diets, deprives the body of protein and micronutrients essential for collagen cross-linking and immune function. These factors don’t doom healing, but they narrow the margin for error and make consistent care crucial.
Protein Is the Backbone
Regular, protein-rich meals or supplements support collagen formation and immune resilience.
Micronutrients and Hydration Matter
Vitamin C, zinc, and adequate hydration help cells proliferate and resist infection during the repair process.
Metabolic Paths to Wound Dehiscence
Diabetes compromises healing on several fronts. Elevated glucose blunts immune cell activity, feeds bacteria, stiffens microvasculature, and reduces oxygen delivery at the capillary level. Swinging between highs and lows can be as problematic as persistent elevation, keeping the wound environment in a prolonged state of inflammation. Tight, safe glucose ranges before and after procedures can markedly lower the likelihood of wound dehiscence by restoring the cellular choreography required for orderly closure.
Medications That Nudge Toward Wound Dehiscence
Several common drugs nudge the biology of healing in the wrong direction. The goal is not to stop essential medications, but to recognize their effects and plan compensations with a clinician’s guidance.
Steroids and Immunosuppressants
They dampen inflammation but also slow fibroblast activity and collagen deposition, weakening early strength.
Chemotherapy and Chronic NSAID Use
Cytotoxic agents and long-term anti-inflammatory regimens can impair cell turnover and platelet function at the wound site.
Lifestyle Risks for Wound Dehiscence
Nicotine narrows blood vessels and reduces oxygen delivery, while carbon monoxide binds hemoglobin and further limits tissue oxygenation. Together, they create a hypoxic microenvironment that invites wound dehiscence. Excessive alcohol use depletes nutrients, suppresses immunity, and increases accidental trauma to a healing site. Pausing nicotine products before and after surgery and moderating alcohol intake provide a measurable bump in tensile strength as the incision matures.
Wound Dehiscence Triggered by Cough, Vomit, or Straining
Abdominal incisions face unique mechanical forces. A single bout of forceful coughing, retching, or straining can spike intra-abdominal pressure and pry at suture lines that are still weak.
Support Reduces Strain
Abdominal binders, cough-splinting with a pillow, and early control of nausea protect healing tissue.
Prevent the Push
Stool softeners, hydration, and fiber reduce constipation so the incision isn’t stressed on the toilet.
The Impact of Body Composition on Wound Dehiscence
Excess adipose tissue is less vascular, resulting in lower oxygen tension and increased dead space that can accumulate fluid. Shear forces are higher, dressings are harder to secure, and comorbidities like sleep apnea raise coughing and pressure swings. On the other hand, underweight patients may lack the protein reserves to build robust collagen. Both extremes increase susceptibility to wound dehiscence; however, thoughtful planning—such as secure closures, appropriate drain use, nutrition support, and tailored activity limits—can help offset the risk.
Wound Dehiscence Linked to Hypothermia During Surgery
Operating room conditions matter. Prolonged procedures raise the odds of tissue drying and contamination. Mild hypothermia slows enzymatic reactions necessary for clotting and collagen assembly. Emergency surgeries often begin with less optimal conditions—dehydration, infection, or unstable hemodynamics—stacking the deck against clean, efficient repair. Proactive warming, moisture-preserving techniques, and stabilization before incision, when feasible, all reduce downstream wound dehiscence.
Hematomas and Fluid Pockets Setting Up Wound Dehiscence
Blood or serous fluid trapped near the incision separates tissue planes and feeds bacteria. As pressure builds, oxygen levels drop, and sutures cut through softened tissue, the risk of wound dehiscence increases.
Drains and Compression Have a Role
When indicated, temporary drains and well-fitted compression garments reduce the space where fluid can pool.
Watch the Contours
Sudden swelling, firmness, or fluctuant areas warrant prompt evaluation before they undermine closure.
Wound Dehiscence Prevention in High-Risk Tissue Environments
Irradiated skin heals more slowly due to microvascular damage, fibrosis, and reduced cell turnover. Incisions through old scars face similar challenges: disorganized collagen and limited elasticity create zones that don’t distribute force evenly. In both scenarios, layered closures, careful tension management, and more extended protection periods can lower the likelihood of wound dehiscence while the tissue gradually regains strength.
Daily Habits That Prevent Wound Dehiscence
After you leave the clinic, routine becomes the safeguard. Clean hands, gentle rinsing, and moisture-balancing dressings keep the microenvironment favorable. Movement is not the enemy; controlled mobility improves circulation and helps prevent clots. What matters is avoiding sudden, high-load motions that yank at the line. Scheduled follow-ups provide checkpoints to adjust materials, address pain, and spot early warning signs before they tip into wound dehiscence.
Protect, Then Mobilize.
Short walks, careful transfers, and good body mechanics feed the wound without overstressing it.
Know When to Call.
Increasing pain, odor, fever, or gaps at the edges are signs to be addressed promptly.
Fragile Skin States and Their Tie to Wound Dehiscence
Long-term topical or systemic steroids thin the dermis and reduce tensile strength. Connective tissue disorders like Ehlers-Danlos change collagen structure, making it more prone to stretching and tearing. Sun-damaged areas may be stiffer and less compliant. Recognizing fragile skin ahead of time leads to strategies—gentle handling, wider suture bites, non-adherent dressings—that keep edges approximated and reduce the chance of wound dehiscence during the early, vulnerable days.
Recognizing Wound Dehiscence Before It Widens
Small signals often precede separation. A sudden “pop” sensation with clear or blood-tinged drainage, edges that look shiny and pulled apart, increasing discomfort after a plateau, or a new smell are all concerning. In abdominal cases, any visible deep tissue or a gush of fluid is an emergency. Photographing the site every few days can make subtle changes obvious. Acting on these clues early can prevent a struggling incision from progressing to wound dehiscence, which requires re-closure.
Pain Control That Protects Against Wound Dehiscence
Pain changes behavior, and behavior changes healing. If dressing changes sting, people delay them; if movement hurts, they avoid it, and circulation suffers. Pre-soaking adherent dressings, choosing non-adherent contact layers, timing changes with prescribed analgesics, and using gentle counter-pressure around—not on—the incision reduces dread and promotes consistency. That steadiness is a quiet antidote to wound dehiscence because closures fail more often when care becomes sporadic.
Simple, Practical Steps to Keep Wound Dehiscence at Bay
Prehab—small steps before surgery—pays dividends afterward. Improving glucose control, pausing nicotine use, optimizing protein intake, and arranging for home support can lower the risk. After the procedure, keep the area clean and moist (not wet), support it during coughs, and follow lifting restrictions. Protect the site from friction at waistbands or straps, and keep pets and curious fingers away. These modest habits collectively raise early tensile strength, narrowing the window where wound dehiscence is most likely.
Adjuncts That Lower Wound Dehiscence Risk
In selected patients, adjuncts such as negative pressure dressings over closed incisions, retention sutures in high-tension zones, or prophylactic antibiotics for contaminated fields can reduce complications. None replace basics like meticulous technique and good home routines; they add a safety margin when biology or biomechanics are less forgiving. The best results come from matching the tool to the risk profile rather than applying the same recipe to every case of wound dehiscence risk.
The Many Small Levers, Big Results Of Wound Dehiscence
Separation rarely stems from a single factor. It is usually the end result of micro-stresses on the line, slower-than-expected biology, and care gaps that accumulate. The encouraging takeaway is that many levers are within reach. By balancing tension, protecting blood flow, controlling infection, fueling the body, and adhering to a clear routine, patients and clinicians can decisively shift the odds toward a quiet, uneventful close. The more these fundamentals are honored, the less likely wound dehiscence becomes—and the sooner life returns to normal.
Visit the Stem Health Plus LLC blog to learn more about how to prevent wound dehiscence and improve your health.
